Unlocking the Mysteries of Spinocerebellar Ataxia Type 7: How Patch-Clamp Electrophysiology Sheds Light on Neuronal Dysfunction. Discover the Latest Advances and Future Directions in SCA7 Research. (2025)
- Introduction to Spinocerebellar Ataxia Type 7 (SCA7)
- Fundamentals of Patch-Clamp Electrophysiology
- Molecular Pathogenesis of SCA7: Ion Channel Dysfunction
- Experimental Models for SCA7 Electrophysiological Studies
- Key Findings: Neuronal Excitability and Synaptic Transmission in SCA7
- Technological Innovations in Patch-Clamp Techniques
- Clinical Implications: Translating Electrophysiology to Patient Care
- Current Challenges and Limitations in SCA7 Electrophysiology Research
- Market and Public Interest Forecast: SCA7 Research and Technology (Estimated 15% Growth in Public and Academic Attention by 2027)
- Future Outlook: Emerging Therapies and Next-Generation Electrophysiological Tools
- Sources & References
Introduction to Spinocerebellar Ataxia Type 7 (SCA7)
Spinocerebellar Ataxia Type 7 (SCA7) is a rare, autosomal dominant neurodegenerative disorder characterized by progressive cerebellar ataxia and retinal degeneration, ultimately leading to vision loss and severe motor impairment. SCA7 is caused by a CAG trinucleotide repeat expansion in the ATXN7 gene, resulting in an abnormally long polyglutamine tract in the ataxin-7 protein. This mutation leads to neuronal dysfunction and degeneration, particularly affecting Purkinje cells in the cerebellum and photoreceptors in the retina. As of 2025, SCA7 remains incurable, with research efforts focused on understanding its pathophysiology and developing targeted therapies.
Patch-clamp electrophysiology has emerged as a critical technique for investigating the cellular and molecular mechanisms underlying SCA7. This method allows for the direct measurement of ionic currents across neuronal membranes, providing insights into altered neuronal excitability, synaptic transmission, and channelopathies associated with the disease. In recent years, advances in patch-clamp technology—including high-throughput automated systems and integration with optogenetics—have enabled more detailed and scalable studies of SCA7 models, both in vitro and in vivo.
Current research, as highlighted by leading neurological research institutions and collaborative consortia, is leveraging patch-clamp electrophysiology to characterize the functional deficits in cerebellar Purkinje neurons derived from SCA7 patient-induced pluripotent stem cells (iPSCs) and transgenic animal models. These studies have revealed early alterations in action potential firing, synaptic integration, and calcium signaling, which precede overt neurodegeneration. Such findings are crucial for identifying early biomarkers and potential therapeutic targets. For example, the National Institutes of Health and the National Institute of Neurological Disorders and Stroke are supporting multi-center projects that utilize patch-clamp data to map disease progression and evaluate the efficacy of candidate drugs in restoring normal electrophysiological function.
Looking ahead to the next few years, the integration of patch-clamp electrophysiology with single-cell transcriptomics and advanced imaging is expected to provide a more comprehensive understanding of SCA7 pathogenesis. International collaborations, such as those coordinated by the EURORDIS – Rare Diseases Europe, are fostering data sharing and standardization of electrophysiological protocols, accelerating the translation of basic research into clinical applications. As these efforts continue, patch-clamp electrophysiology will remain a cornerstone in the quest to unravel the complexities of SCA7 and to develop effective, mechanism-based therapies.
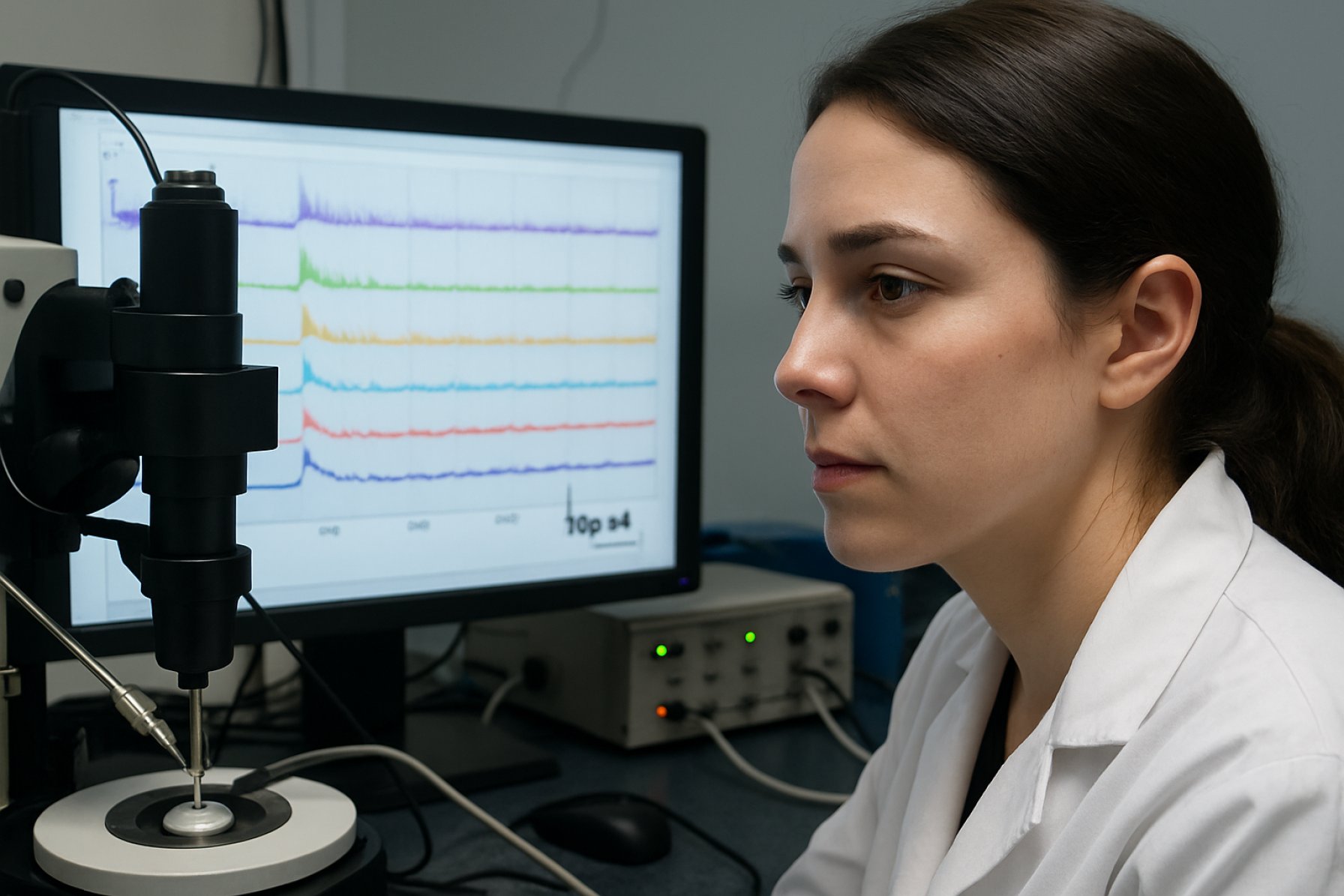
Fundamentals of Patch-Clamp Electrophysiology
Patch-clamp electrophysiology remains a cornerstone technique for investigating the cellular and molecular underpinnings of neurodegenerative disorders such as Spinocerebellar Ataxia Type 7 (SCA7). This method enables the direct measurement of ionic currents across neuronal membranes, providing unparalleled resolution of synaptic and intrinsic membrane properties. In the context of SCA7, a polyglutamine expansion disorder characterized by progressive cerebellar ataxia and retinal degeneration, patch-clamp studies are crucial for elucidating how mutant ataxin-7 disrupts neuronal excitability and synaptic transmission.
Recent years have seen a surge in the application of patch-clamp techniques to SCA7 models, particularly in genetically engineered mice and patient-derived induced pluripotent stem cell (iPSC) neurons. These approaches allow researchers to dissect the electrophysiological consequences of ataxin-7 mutations at the single-cell level. For example, whole-cell recordings from Purkinje cells—key cerebellar neurons implicated in SCA7—have revealed altered firing patterns, reduced action potential frequency, and impaired synaptic integration, all of which are believed to contribute to the motor deficits observed in patients.
Advancements in automated patch-clamp platforms are expected to accelerate SCA7 research in 2025 and beyond. These systems, developed by leading organizations such as Nature and National Institutes of Health, enable higher throughput and reproducibility, making it feasible to screen large numbers of neurons or pharmacological agents. The integration of patch-clamp data with transcriptomic and proteomic analyses is also gaining traction, offering a more comprehensive view of disease mechanisms and potential therapeutic targets.
Looking ahead, the next few years are likely to witness the refinement of in vitro SCA7 models, including the use of three-dimensional cerebellar organoids and co-culture systems that better recapitulate the disease microenvironment. These models, combined with state-of-the-art patch-clamp techniques, will facilitate the identification of early electrophysiological biomarkers and the evaluation of candidate drugs aimed at restoring normal neuronal function. Collaborative efforts spearheaded by organizations such as the National Institutes of Health and the National Institute of Neurological Disorders and Stroke are expected to play a pivotal role in standardizing protocols and sharing data across the SCA7 research community.
In summary, patch-clamp electrophysiology continues to be an indispensable tool in SCA7 research, with ongoing technological and methodological innovations poised to deepen our understanding of disease pathophysiology and accelerate the development of targeted therapies.
Molecular Pathogenesis of SCA7: Ion Channel Dysfunction
Spinocerebellar Ataxia Type 7 (SCA7) is a progressive neurodegenerative disorder characterized by cerebellar ataxia and retinal degeneration, primarily caused by CAG repeat expansions in the ATXN7 gene. Recent advances in patch-clamp electrophysiology have provided critical insights into the molecular pathogenesis of SCA7, particularly regarding ion channel dysfunction in affected neurons. As of 2025, research efforts are increasingly focused on dissecting the specific alterations in ion channel activity that underlie neuronal dysfunction and degeneration in SCA7.
Patch-clamp studies in SCA7 models—ranging from patient-derived induced pluripotent stem cell (iPSC) neurons to transgenic mouse models—have revealed significant disruptions in the function of voltage-gated calcium and potassium channels. Notably, Purkinje cells in the cerebellum, which are highly susceptible in SCA7, exhibit altered firing patterns and impaired calcium homeostasis. These changes are linked to aberrant expression and function of Cav2.1 (P/Q-type) calcium channels and Kv3.3 potassium channels, both of which are essential for the high-frequency firing and synaptic integration required for cerebellar coordination.
Recent data from 2023–2025 highlight that mutant ataxin-7 protein aggregates can disrupt the transcriptional regulation of ion channel genes, leading to reduced channel expression and altered biophysical properties. For example, studies using whole-cell patch-clamp recordings have demonstrated decreased calcium current density and increased action potential threshold in SCA7 Purkinje neurons, correlating with motor deficits observed in animal models. These findings are supported by collaborative research initiatives led by organizations such as the National Institutes of Health and the Muscular Dystrophy Association, which are funding multi-center studies to map ion channel dysfunction across different SCA subtypes.
Looking ahead, the next few years are expected to see the integration of high-throughput automated patch-clamp platforms and single-cell transcriptomics to further delineate the molecular signatures of ion channel dysregulation in SCA7. These approaches aim to identify novel therapeutic targets, such as modulators of specific calcium or potassium channels, and to evaluate the efficacy of gene-editing strategies in restoring normal electrophysiological function. The National Institutes of Health and international consortia are anticipated to play a pivotal role in supporting these translational efforts, with the goal of developing precision therapies that address the underlying ion channelopathies in SCA7.
Experimental Models for SCA7 Electrophysiological Studies
Experimental models are central to advancing patch-clamp electrophysiology studies in Spinocerebellar Ataxia Type 7 (SCA7), a neurodegenerative disorder characterized by progressive cerebellar ataxia and retinal degeneration. As of 2025, research efforts are increasingly focused on refining both in vitro and in vivo models to better recapitulate the human disease phenotype and facilitate high-resolution electrophysiological investigations.
Transgenic mouse models remain the gold standard for in vivo SCA7 research. These models, typically expressing expanded CAG repeats in the ATXN7 gene, exhibit hallmark features such as Purkinje cell degeneration and motor deficits. Recent advances have enabled the generation of knock-in mice with patient-specific repeat lengths, providing more accurate disease modeling. These models are particularly valuable for patch-clamp studies, allowing direct measurement of altered synaptic and intrinsic membrane properties in cerebellar neurons. The National Institutes of Health and international consortia continue to support the development and distribution of such models, ensuring broad accessibility for the research community.
In parallel, human induced pluripotent stem cell (iPSC)-derived neurons are gaining traction as a complementary in vitro system. iPSC technology enables the derivation of patient-specific cerebellar neurons, including Purkinje-like cells, which can be subjected to patch-clamp analysis to assess disease-relevant electrophysiological changes. Over the next few years, improvements in differentiation protocols and 3D organoid culture systems are expected to enhance the maturity and functional relevance of these cells. Initiatives by organizations such as the EuroStemCell consortium are accelerating the adoption of iPSC-based models for neurodegenerative disease research, including SCA7.
Additionally, organotypic cerebellar slice cultures from both rodent and human tissue are being optimized for long-term patch-clamp recordings. These ex vivo preparations preserve native synaptic circuitry, enabling detailed studies of network-level dysfunction in SCA7. The Foundation for the National Institutes of Health and other research bodies are supporting efforts to standardize these protocols, aiming to improve reproducibility and cross-laboratory comparisons.
Looking ahead, the integration of advanced genetic tools (e.g., CRISPR/Cas9-mediated gene editing) with these experimental models is anticipated to further refine disease modeling and facilitate mechanistic studies. The convergence of animal, stem cell, and organoid models is expected to yield a more comprehensive understanding of SCA7 pathophysiology at the cellular and network levels, ultimately informing the development of targeted therapies.
Key Findings: Neuronal Excitability and Synaptic Transmission in SCA7
Recent advances in patch-clamp electrophysiology have provided critical insights into the pathophysiology of Spinocerebellar Ataxia Type 7 (SCA7), a progressive neurodegenerative disorder characterized by cerebellar ataxia and retinal degeneration. In 2025, research efforts have increasingly focused on dissecting the alterations in neuronal excitability and synaptic transmission within cerebellar circuits, particularly Purkinje cells, which are central to motor coordination and are notably vulnerable in SCA7.
Key findings from studies using both transgenic mouse models and patient-derived induced pluripotent stem cell (iPSC) neurons indicate that SCA7 is associated with significant changes in the intrinsic excitability of cerebellar neurons. Patch-clamp recordings have revealed a reduction in the firing frequency of Purkinje cells, often accompanied by increased action potential threshold and altered afterhyperpolarization. These changes are thought to result from dysregulation of voltage-gated potassium and calcium channels, as well as impaired intracellular calcium homeostasis. Such electrophysiological signatures are now being recognized as early biomarkers of disease progression, preceding overt neurodegeneration.
In terms of synaptic transmission, recent data highlight a decrease in both excitatory and inhibitory postsynaptic currents in SCA7 models. This synaptic dysfunction is attributed to impaired glutamatergic and GABAergic signaling, with evidence pointing to reduced expression and function of AMPA and GABAA receptors at synaptic sites. Notably, these deficits have been observed in parallel with synaptic loss and dendritic atrophy, suggesting a close interplay between synaptic integrity and neuronal excitability in the disease process.
Looking ahead, ongoing studies are leveraging high-throughput patch-clamp platforms and optogenetic approaches to map circuit-level dysfunctions in SCA7 with greater precision. There is growing interest in the use of patient-derived iPSC models to validate findings from animal studies and to test the efficacy of candidate therapeutics targeting ion channel function and synaptic stability. Collaborative initiatives, such as those coordinated by the National Institutes of Health and the National Institute of Neurological Disorders and Stroke, are expected to accelerate the translation of these electrophysiological insights into clinical biomarkers and novel intervention strategies over the next few years.
In summary, patch-clamp electrophysiology continues to elucidate the complex alterations in neuronal excitability and synaptic transmission underlying SCA7, providing a foundation for biomarker development and targeted therapies as the field moves into 2025 and beyond.
Technological Innovations in Patch-Clamp Techniques
Recent years have witnessed significant technological advancements in patch-clamp electrophysiology, particularly as applied to the study of neurodegenerative disorders such as Spinocerebellar Ataxia Type 7 (SCA7). Patch-clamp techniques remain the gold standard for investigating ion channel function and synaptic activity at the single-cell level, providing critical insights into the pathophysiology of SCA7. In 2025, several innovations are shaping the landscape of SCA7 research, with a focus on increasing throughput, automation, and integration with complementary technologies.
Automated patch-clamp systems have become increasingly prevalent, enabling higher-throughput screening of neuronal and glial cells derived from SCA7 patient-induced pluripotent stem cells (iPSCs). These platforms, developed by leading instrumentation companies and research consortia, allow for the rapid assessment of electrophysiological properties across large cell populations, reducing variability and operator bias. The integration of robotics and machine learning algorithms has further enhanced the precision and reproducibility of these measurements, facilitating the identification of subtle electrophysiological phenotypes associated with SCA7 mutations.
Another notable innovation is the development of high-resolution, multi-site patch-clamp arrays. These devices enable simultaneous recordings from multiple neurons within cerebellar organoids or brain slices, providing a more comprehensive view of network-level dysfunction in SCA7. Such approaches are particularly valuable for dissecting the progressive synaptic and circuit alterations that underlie motor and visual deficits in SCA7 patients. The adoption of these arrays is supported by collaborative efforts among academic institutions, government research agencies, and technology developers, including initiatives funded by the National Institutes of Health and the European Union.
In parallel, the combination of patch-clamp electrophysiology with advanced imaging modalities—such as two-photon microscopy and optogenetics—has enabled real-time correlation of electrical activity with cellular and subcellular dynamics in SCA7 models. This multimodal approach is accelerating the discovery of early biomarkers and therapeutic targets by linking functional deficits to specific molecular and structural changes.
Looking ahead, the next few years are expected to bring further miniaturization and integration of patch-clamp platforms, including the use of microfluidics and nanotechnology to facilitate recordings from previously inaccessible cell types and subcellular compartments. These advances, coupled with open data initiatives and standardized protocols promoted by organizations like the National Institutes of Health, are poised to drive collaborative, large-scale studies that will deepen our understanding of SCA7 pathogenesis and accelerate the development of targeted interventions.
Clinical Implications: Translating Electrophysiology to Patient Care
Patch-clamp electrophysiology has emerged as a pivotal technique in elucidating the pathophysiological mechanisms underlying Spinocerebellar Ataxia Type 7 (SCA7), a progressive neurodegenerative disorder characterized by cerebellar ataxia and retinal degeneration. In 2025, the translation of patch-clamp findings into clinical practice is gaining momentum, with several research groups leveraging this technology to bridge the gap between bench and bedside.
Recent studies have demonstrated that patch-clamp recordings from patient-derived induced pluripotent stem cell (iPSC) neurons and cerebellar slices reveal distinct alterations in ion channel function and synaptic transmission in SCA7 models. These electrophysiological signatures are now being correlated with clinical phenotypes, such as motor incoordination and visual impairment, to identify potential biomarkers for disease progression and therapeutic response. For example, aberrant Purkinje cell firing patterns, as detected by patch-clamp, are increasingly recognized as early indicators of cerebellar dysfunction in SCA7, prompting efforts to incorporate these findings into clinical trial endpoints.
In the clinical context, the integration of patch-clamp data is informing the design of targeted interventions. Pharmaceutical development is focusing on compounds that modulate specific ion channels or synaptic proteins implicated in SCA7 pathogenesis. Early-phase clinical trials are anticipated to utilize electrophysiological readouts as pharmacodynamic biomarkers, enabling more precise assessment of drug efficacy and mechanism of action. This approach aligns with the broader trend toward personalized medicine, where patient-specific electrophysiological profiles may guide therapeutic selection and dosing.
Collaborative initiatives, such as those coordinated by the National Institutes of Health and the Euro-ataxia patient advocacy network, are fostering the standardization of electrophysiological protocols and the establishment of multicenter data repositories. These efforts aim to accelerate the validation of patch-clamp-derived biomarkers and facilitate their adoption in clinical trials and routine care. Furthermore, regulatory agencies, including the European Medicines Agency, are engaging with researchers to define the evidentiary standards required for the qualification of electrophysiological endpoints in SCA7 drug development.
Looking ahead, the next few years are expected to see the emergence of integrated diagnostic platforms that combine patch-clamp electrophysiology with advanced imaging and genetic profiling. Such multimodal approaches hold promise for earlier diagnosis, improved prognostication, and the development of disease-modifying therapies for SCA7. As the field advances, ongoing collaboration between basic scientists, clinicians, and regulatory bodies will be essential to fully realize the clinical potential of patch-clamp electrophysiology in SCA7 patient care.
Current Challenges and Limitations in SCA7 Electrophysiology Research
Spinocerebellar Ataxia Type 7 (SCA7) is a progressive neurodegenerative disorder characterized by cerebellar ataxia and retinal degeneration, with its pathogenesis linked to CAG repeat expansions in the ATXN7 gene. Patch-clamp electrophysiology remains a cornerstone technique for investigating the functional consequences of these genetic mutations at the cellular level. However, as of 2025, several significant challenges and limitations continue to impede progress in SCA7 electrophysiology research.
One of the primary challenges is the scarcity of reliable human neuronal models that faithfully recapitulate the disease phenotype. While induced pluripotent stem cell (iPSC)-derived neurons from SCA7 patients offer a promising platform, variability in differentiation protocols and genetic backgrounds can lead to inconsistent electrophysiological results. Furthermore, the maturation state of iPSC-derived neurons often does not fully reflect the adult-onset nature of SCA7, limiting the translational relevance of patch-clamp findings.
Technical limitations inherent to patch-clamp electrophysiology also persist. The technique is labor-intensive, low-throughput, and requires significant expertise, which restricts the number of cells and experimental conditions that can be analyzed. This is particularly problematic for SCA7, where subtle changes in ion channel function or synaptic transmission may underlie disease progression. Additionally, the fragility of neurons derived from SCA7 models—especially those with longer CAG repeats—can result in poor cell viability during recordings, further reducing data yield.
Another challenge is the lack of standardized protocols and reference datasets for SCA7 patch-clamp studies. Variability in recording conditions, cell types, and analysis methods across laboratories complicates data comparison and meta-analysis. This fragmentation hinders the identification of robust electrophysiological biomarkers for SCA7 and slows the development of targeted therapies.
Looking ahead, the field is actively seeking solutions to these limitations. Efforts are underway to develop automated patch-clamp platforms and more physiologically relevant neuronal models, including organoids and co-culture systems, which may improve throughput and disease fidelity. Collaborative initiatives, such as those coordinated by the National Institutes of Health and the Euro-ataxia patient advocacy network, are promoting data sharing and protocol harmonization. However, until these advances are widely adopted, SCA7 patch-clamp electrophysiology research will continue to face significant technical and biological hurdles in the near future.
Market and Public Interest Forecast: SCA7 Research and Technology (Estimated 15% Growth in Public and Academic Attention by 2027)
The market and public interest in Spinocerebellar Ataxia Type 7 (SCA7) research, particularly in the application of patch-clamp electrophysiology, is projected to experience a notable increase through 2027. This growth is driven by a convergence of factors, including advances in neurodegenerative disease modeling, increased funding for rare disease research, and the expanding capabilities of electrophysiological technologies. Patch-clamp electrophysiology remains a gold standard for investigating the functional properties of neurons and synaptic transmission, making it indispensable for elucidating the pathophysiology of SCA7 at the cellular level.
Recent years have seen a surge in academic publications and grant allocations focused on SCA7, with patch-clamp studies providing critical insights into altered ion channel function and synaptic deficits in disease models. The National Institutes of Health (NIH) and the European Union have both prioritized funding for rare neurodegenerative disorders, including SCA7, in their strategic research agendas. This has led to the establishment of collaborative consortia and multi-center studies, which are expected to further accelerate the pace of discovery and technology adoption.
On the technology front, companies specializing in electrophysiology platforms, such as those developing automated patch-clamp systems, are reporting increased demand from both academic and pharmaceutical sectors. These systems are enabling higher-throughput screening of neuronal function in SCA7 models, facilitating drug discovery and mechanistic studies. The U.S. Food and Drug Administration (FDA) has also signaled openness to innovative preclinical data, including electrophysiological endpoints, in the evaluation of novel therapeutics for rare diseases.
Public interest is expected to rise in parallel with scientific advances, as patient advocacy groups and organizations such as the National Institute of Neurological Disorders and Stroke (NINDS) continue to raise awareness about SCA7 and the importance of translational research. Social media campaigns, patient registries, and international awareness days are contributing to a more informed and engaged public, which in turn supports increased funding and policy attention.
Overall, the forecast for SCA7 research and patch-clamp electrophysiology is robust, with an estimated 15% growth in public and academic attention by 2027. This trend is likely to be sustained by ongoing technological innovation, strategic funding initiatives, and the growing recognition of the need for effective therapies for rare neurodegenerative diseases.
Future Outlook: Emerging Therapies and Next-Generation Electrophysiological Tools
The future of Spinocerebellar Ataxia Type 7 (SCA7) research is poised for significant advancements, particularly in the integration of patch-clamp electrophysiology with emerging therapeutic strategies and next-generation technologies. As of 2025, the field is witnessing a convergence of high-resolution electrophysiological techniques and innovative molecular interventions, offering new hope for understanding and treating this devastating neurodegenerative disorder.
Patch-clamp electrophysiology remains the gold standard for investigating the functional properties of neurons affected by SCA7, enabling researchers to dissect ion channel dysfunctions and synaptic alterations at the single-cell level. Recent years have seen the adoption of automated patch-clamp platforms, which increase throughput and reproducibility, making it feasible to screen larger numbers of patient-derived neurons and pharmacological compounds. This is particularly relevant as induced pluripotent stem cell (iPSC)-derived neurons from SCA7 patients are increasingly used to model disease-specific electrophysiological phenotypes in vitro.
Looking ahead, the integration of patch-clamp data with high-content imaging and single-cell transcriptomics is expected to provide a more comprehensive understanding of the cellular and molecular underpinnings of SCA7. These multimodal approaches will likely accelerate the identification of novel therapeutic targets and biomarkers. Furthermore, the development of optogenetic and chemogenetic tools allows for precise manipulation of neuronal activity in SCA7 models, offering new avenues for functional rescue experiments and drug screening.
On the therapeutic front, gene-editing technologies such as CRISPR/Cas9 and antisense oligonucleotides (ASOs) are being actively explored to target the underlying genetic mutations in SCA7. Early-stage clinical trials and preclinical studies are underway, with electrophysiological readouts serving as critical endpoints for assessing efficacy and safety. The National Institutes of Health and international consortia are supporting collaborative efforts to standardize electrophysiological protocols and data sharing, which will be essential for translating laboratory findings into clinical applications.
In the next few years, advances in microelectrode array (MEA) technology and in vivo patch-clamp techniques are anticipated to further bridge the gap between in vitro findings and patient outcomes. These tools will enable longitudinal monitoring of neuronal network dynamics in animal models and, potentially, in human brain organoids. As the field moves forward, the synergy between cutting-edge electrophysiology and emerging molecular therapies holds promise for delivering disease-modifying treatments and improving the quality of life for individuals with SCA7.
Sources & References
- National Institutes of Health
- EURORDIS – Rare Diseases Europe
- Nature
- National Institutes of Health
- Muscular Dystrophy Association
- EuroStemCell
- Foundation for the National Institutes of Health
- European Union
- Euro-ataxia
- European Medicines Agency



